Health, Regeneration
Welcome and thanks for visiting...

Proper Recovery and Regeneration From and for Training Part II
Introduction
According to Ericsson, it takes about 10 years or 10,000 hours of deliberate practice to develop an athlete’s talent in any field (Ericsson, 1996). Given that this amount of time is a requisite for an athlete to become very proficient and efficient in their sport, the concept of recovery and regeneration plays a vital and critical role in and during this process. As alluded to previously (part 1), regular training actively challenges the natural homeostatic balance of the body to elicit adaptation and performance gains (Main and Landers, 2012).
Recovery and regeneration is the means by which restoration occurs. It is comprised of a network of responses aimed at resolving any disruption (physiological, biochemical, and psychological) to the body from the stressful components of training load and competition.
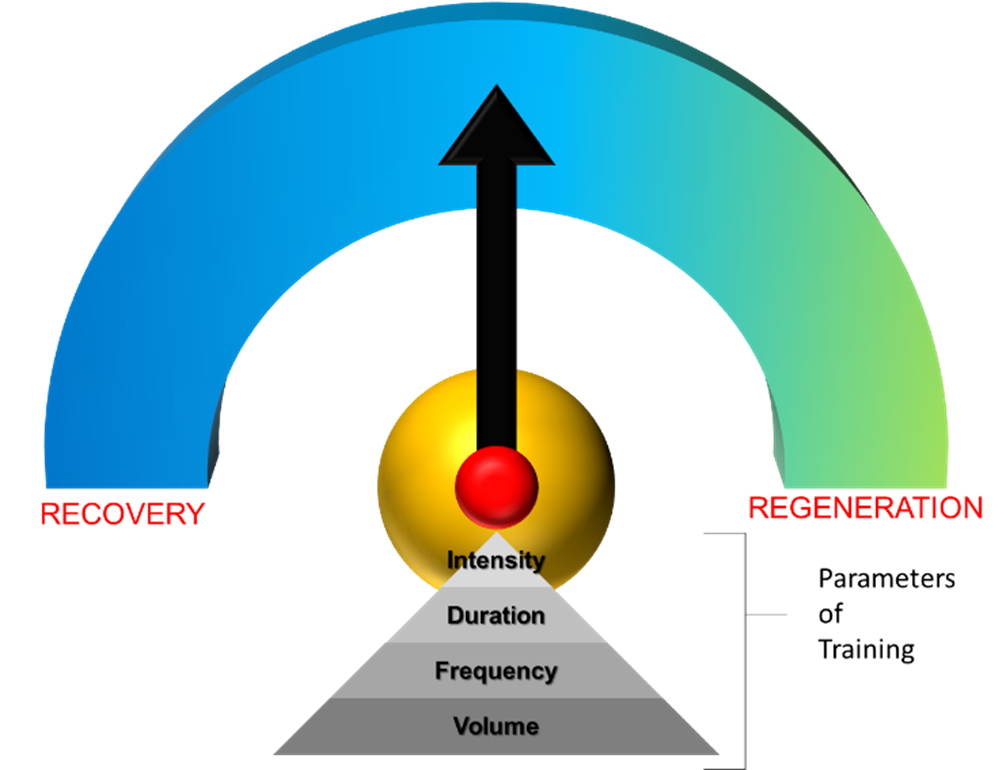
Figure 1 – The Recovery and Regeneration Continuum (copyright © Nikos C. Apostolopoulos 2021)
Although the term recovery and regeneration cites two separate concepts, each being defined by a particular response of the body, either at the micro- or macroscopic level, in reality it is a continuum, dependent upon the parameters of training and adaptation: intensity (how much), duration (how long), frequency (how often), and volume (how much) (figure 1). The manipulation of these parameters allows for the proper dose prescription aiding in the recovery and regeneration of the body.
Recovery
Exercise can be carried out in an incremental or constant manner (endurance), can be dynamic (cycling, running) or static (weightlifting), exhaustive or non-exhaustive, executed under aerobic or anaerobic conditions, with contractions during exercise being isometric, isokinetic, concentric, or eccentric (Finsterer, 2012). Exercise induced changes to muscle force can occur either shortly after the onset of exercise (acute response) or following a constant high-intensity or sub-maximal prolonged period of time (chronic response). Any reduced ability to develop force and power indicates the degree to which muscle dysfunction has been provoked.
Recovery, either passive or active, is the process of addressing this dysfunction to the muscle. It aids in reducing residual fatigue, enabling the athlete to adapt to performance stressors. Since the loss of muscle force due to fatigue is reversible (Rainoldi et al., 2008, Finsterer, 2012), the proper manipulation of the training parameters allows for the creation of a recovery
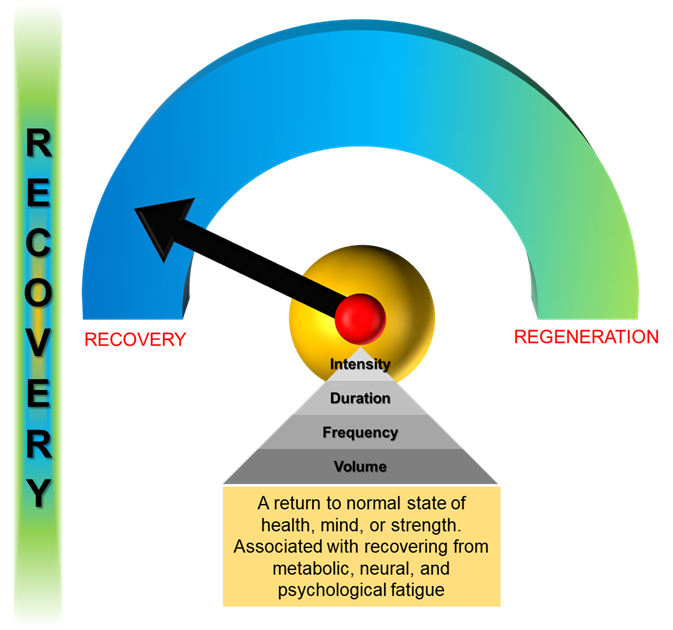
Figure 2 – Recovery (Copyright © Nikos C. Apostolopoulos 2021)
protocol focused on restoring the body’s natural homeostasis. With training arising at the border between adaptation (results of optimal training), and mal-adaptation (excessive training with failure to recover), this protocol ensures that the athlete(s) will have a positive response to the training stimuli, enhancing their ability to tolerate higher training workloads thereby maximizing their performance. Failure to adapt to the training stressors results in harmful conditions such as overtraining (Kentta and Hassmen, 1998), overuse (Aicale et al., 2018), or burnout (Main and Landers, 2012) predisposing the athlete to injury.
As alluded to above, central to the interplay between adaptation and mal-adaptation are various stages (acute or chronic) of fatigue, each associated with physiological and psychological stressors as antecedents of each level. The reduced ability to develop force and power, as well as the sensation of tiredness, reflects the rate of effect of fatigue on muscle function. Below are three types of fatigue each indicating their effect and influence on the athlete and their training (Calder, 2010):
- Metabolic – This refers to the cumulative depletion of the energy stores of the body. This type of fatigue develops when compounds in the body needed to produce adenosine tri-phosphate (ATP) are depleted or when by-products of metabolism accumulate in muscle (Hargreaves, 2005). With metabolic fatigue, the athlete becomes weary sooner than normal, struggling to complete a session or event (Maughan, 2000).
- Neural – This is concerned with fatigue of either or both the peripheral (PNS) and central (CNS) nervous systems, affecting the muscles and brain, respectively (Sayers, 1993, Garrandes et al., 2005). A fatigue of the PNS is associated with reduced localized force production due to a decrease in motor unit firing frequency (Gabriel et al., 2001), with the lack of drive being associated with the CNS (Finsterer, 2012)
- Psychological – This refers to stressors, within and outside of training, such as competition pressure, home, school, and family life, compromising an athlete’s ability to maintain a natural homeostatic balance (Hooper et al., 1999, Main and Landers, 2012). Evidence suggests that psychological processes and emotional states influence the vulnerability to illness (McEwen, 2007)
Regeneration
Regeneration refers to the process or processes of remodelling of the connective and muscle tissues and cells in response to an external force (figure 3). Unlike recovery, which is associated with fatigue, defined as a reversible loss of muscle force (muscle contractility) during work over time (Gosker and Schols, 2008, Rainoldi et al., 2008, Finsterer, 2012), regeneration is concerned with damage to the myofibrillar structure of muscle. This damage rapidly activates multiple cellular and molecular processes fixated on restoring normal muscle structure and function (Nedjar, 2011, Philipou et al., 2012, Heisenberg and Bellaiche, 2013). A consequence of this disturbance is the interaction(s) between skeletal muscle damage and the consequent inflammatory response (Philipou et al., 2012), an interaction dependent upon the intensity and duration of the stimulus (Tidball, 2011).
As mentioned in part 1, a bout of strenuous physical activity may cause substantial tissue injury, inducing a rapid yet complex sequence of immune reactions, and a secondary immunosuppression (Northoff et al., 1995, Shephard and Shek, 1998a). Although the inflammatory response is subclinical (athlete recovers fully) (Shephard and Shek, 1998b, Shephard, 2001), the active interaction of the skeletal muscle with the immune system responds by secreting various pro- and anti-inflammatory proteins regulating multiple biological processes promoting the resolution of muscle tissue and its cells.
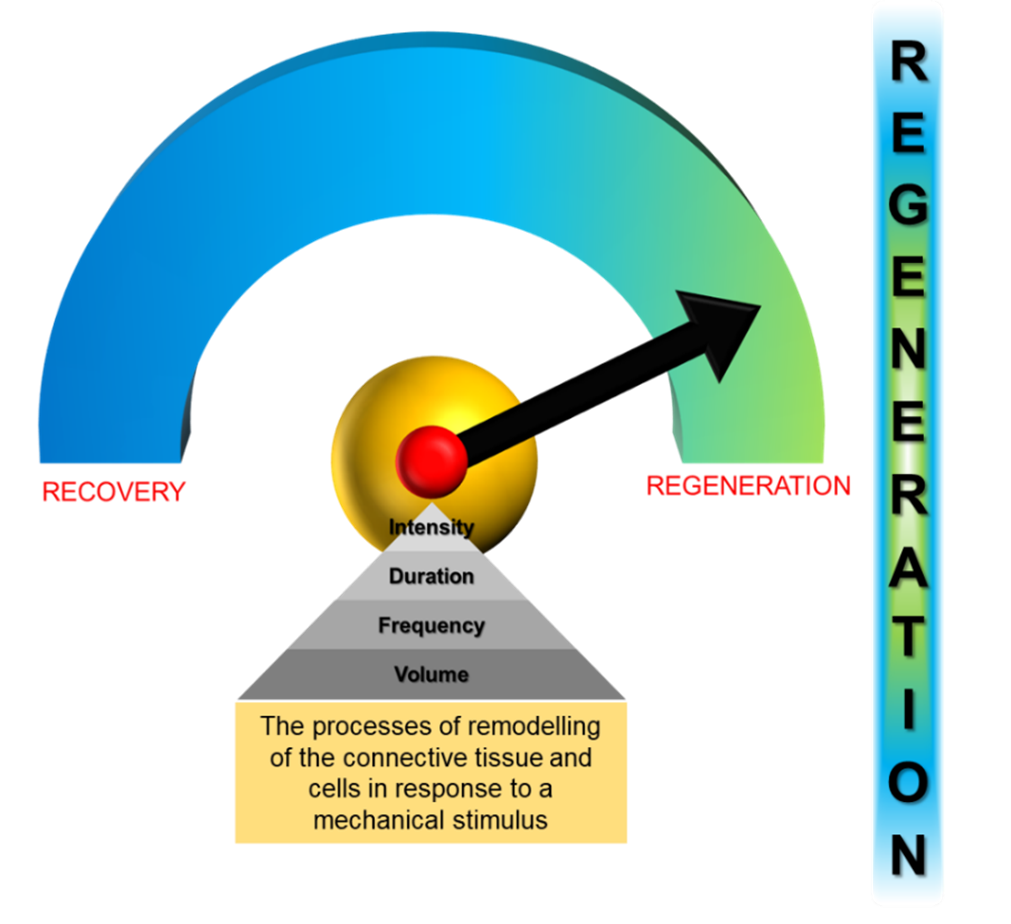
Figure 3 – Regeneration (copyright © Nikos C. Apostolopoulos)
The injury to the tissue is responsible for inducing the rehabilitation of its structural environment in order to return to its normal resting tension that is typically built into the anatomy of the tissue(s) (Gerarduzzi and Di Battista, 2017). Regeneration accomplishes this by the release of several growth factors ensuring the reconstruction of the original internal structure of the tissue and scaffold, enabling it to again take over and respond appropriately to the mechanical load of the tissue (Tomasek et al., 2002). In otherwords, regeneration fulfils the ability to rehabilitate the tissue in order to handle the magnitude and the distribution of forces generated during training.
Similar to recovery, the appropriate manipulation of the training parameters is key to mitigating the inflammatory response thereby aiding in the restitution of the tissue and the re-establishment of the homeostasis of the body (Apostolopoulos, 2018). Research has observed that the proper prescription of intensity, duration, and frequency was responsible for the decrease in muscle soreness as well as an increase in muscle function following delayed onset muscle soreness (Apostolopoulos et al., 2018).
Conclusion
The term recovery and regeneration refers to two separate concepts, associated with distinct responses concerning the response of the body to training and competition. The former is seen as the process of preparing the athlete to tolerate more frequent and intense training by improving their ability to adapt both physically and psychologically, while the latter is concerned with the mending of the tissue(s) in response to any mechanical stimulus. It is a highly orchestrated process characterized by inflammation, the degeneration of the damaged tissue, and the release of growth factors guiding muscle regeneration. However, what is common amongst both is their intricate interrelationship designed to re-establish the natural homeostasis of the body over time. To achieve this, coaches, trainers, and clinicians can design recovery and regeneration protocols based on the manipulation of the training parameters: intensity, duration, frequency, and volume.
Read more:
Proper Recovery and Regeneration From and for Training Part I
REFERENCES
AICALE, R., TARANTINO, D. & MAFFULLI, N. 2018. Overuse injruies in sport: a comprehensive overview. J Orth Surg Res, 13, 1-11.
APOSTOLOPOULOS, N. C. 2018. Stretch intensity and the Inflammatory Response: A Paradigm Shift Switzerland, Springer-Nature.
APOSTOLOPOULOS, N. C., LAHART, I. M., PLYLEY, M. J., TAUNTON, J., NEVILL, A. M., KOUTEDAKIS, Y., WYON, M. & METSIOS, G. S. 2018. The effects of different passive static stretching intensities on recovery from unaccustomed eccentric exercise - a randomized controlled trial. Appl Physiol Nutr Metab, 43, 806-15.
CALDER, A. 2010. The scientific basis for recovery training practices in sport. Int J Sports Sci Phys Educ 1, 43-9.
ERICSSON, K. A. 1996. The road to excellence: The acquisition of expert performance in the arts and sciences, sports and games, Mahwah, NJ, Erlbaum.
FINSTERER, J. 2012. Biomarkers of peripheral muscle fatigue during exercise. BMC Musculoskeletal Disorders, 13, 1-13.
GABRIEL, D. A., BASFORD, J. R. & AN, K.-N. 2001. Neural adaptations to fatigue: implications for muscle strength and training. Med Sci Sports Exerc, 33, 1354-60.
GARRANDES, F., COLSON, S. S., PENSINI, M. & LEGROS, P. 2005. Neuromuscular fatigue kinetics are sport specific. Comp Meth Biomech Biomed Enging, 113-4.
GERARDUZZI, C. & DI BATTISTA, J. A. 2017. Nyofibroblast repair mechanisms post-inflammatory response: a fibrotic perspective. Inflamm Res, 66, 451-65.
GOSKER, H. R. & SCHOLS, A. M. 2008. Fatigued muscles in COPD but no finishing line in sight. Eur Respir J, 31, 693-4.
HARGREAVES, M. 2005. Metabolic factors in fatigue. Sports Sci Exchange 98, 18, 1-9.
HEISENBERG, C.-P. & BELLAICHE, Y. 2013. Forces in tissue morphogenesis and patterning. Cell, 153, 948-62.
HOOPER, S. L., MACKINNON, L. T. & HOWARD, A. 1999. Physiological and psyhometric variables for monitoring overtraing and recovery. Int J Sports Psych, 28, 1-12.
KENTTA, G. & HASSMEN, P. 1998. Overtraining and Recovery A Conceptual Model. Sports Med, 26, 1-16.
MAIN, L. C. & LANDERS, G. J. 2012. Overtraining or burnout: a trainng and psycho-behavioral case study. Int J SPorts Sci Coaching, 7, 23-31.
MAUGHAN, R. (ed.) 2000. Fluid and carbohydrate intake during exercise, Roseville: McGraw Hill.
MCEWEN, B. S. 2007. Physiology and neurobiology of stress and adaptation: Central role of the brain. Physiol Rev, 87, 873-904.
NEDJAR, B. 2011. On a continuum thermodynamics formulation and computational aspects of finite growth in soft tissues. Int J Numer Meth Biomed Engng, 27, 1850-66.
NORTHOFF, H., ENKEL, S. & WEINSTOCK, C. 1995. Exercise, injury and immune function. ExImmunolRev, 1, 1-25.
PHILIPOU, A., MARIDAKI, M., THEOS, A. & KOUTSILIERIS, M. 2012. Cytokines in muscle damage. Adv Clin Chem, 58, 49-87.
RAINOLDI, A., GAZZONI, M., MERELETTI, R. & MINETTO, M. A. 2008. Mechanical and EMG responses of the vastus lateralis and changes in biochemical variables to isokinetic exercise in endurance and power atheltes. J Sports Sci, 26, 321-31.
SAYERS, M. 1993. Neuromuscular fatigue and recovery: a brief review. Strength Cond Coach, 1, 12-14.
SHEPHARD, R. J. 2001. Sepsis and mechanisms of inflammatory response: is exercise a good model? Br J Sports Med, 35, 223-30.
SHEPHARD, R. J. & SHEK, P. N. 1998a. Immune respnses to inflammation and trauma: a physical training model. CanJPhysiolPharmacol, 76, 469-72.
SHEPHARD, R. J. & SHEK, P. N. 1998b. Immune responses to inflammation and trauma: a physical training model. Can J Physiol Pharmacol, 76, 469-72.
TIDBALL, J. G. 2011. Mechanisms of muscle injury, repair, and regeneration. Compr Physiol, 1, 2029-62.
TOMASEK, J. J., GABBIANI, G., HINZ, B., CHAPONNIER, C. & BROWN, R. A. 2002. Myofibroblasts and mechano-regulation o connective tissue remodelling. Nat Rev Mol Cell Biol, 3, 349-63.
Read more:
Proper Recovery and Regeneration From and for Training Part I
Proper Recovery and Regeneration From and for Training Part II
Proper Recovery and Regeneration From and for Training Part III