Welcome and thanks for visiting...

Understanding Insulin Resistance: A Guide for Everyone

To see this video, you must be a member. Membership options:
Free - newsletter, video & blog access,
earn

Yearly - full access & member features
earn 5x

US$179 - may be lower outside US
Lifetime - same as yearly, but forever
earn 10x

US$350 - may be lower outside US
earn

Yearly - full access & member features
earn 5x

US$179 - may be lower outside US
Lifetime - same as yearly, but forever
earn 10x

US$350 - may be lower outside US
MySportsEdTV is a community where people share their passion for sports. It’s a place where athletes, coaches and parents can share information and share experiences. It’s a place to make new friends across the globe. Members have access to great features unavailable to non-members. Members receive helpful information via our FREE email newsletters. We always respect your privacy and your data will not be sold or shared
To use this function, you must be a full member. Membership options:
Free - newsletter, all video & blog access
Yearly - full access & member features
US$179 - may be lower outside US
Lifetime - same as yearly, but forever
US$350 - may be lower outside US
You may also use a promo code for payment
Yearly - full access & member features
US$179 - may be lower outside US
Lifetime - same as yearly, but forever
US$350 - may be lower outside US
You may also use a promo code for payment
MYSportsEdTV is a community where athletes, coaches and parents connect and share their sport passion. We don’t sell our member data or send spam. Members will receive our FREE email newsletter to alert you about new video and blog content for the sports you follow.
To use this function, you must be a paid member. Membership options:
Free - newsletter, all video & blog access
Yearly - full access & member features
US$179 - may be lower outside US
Lifetime - same as yearly, but forever
US$350 - may be lower outside US
You may also use a promo code for payment
Yearly - full access & member features
US$179 - may be lower outside US
Lifetime - same as yearly, but forever
US$350 - may be lower outside US
You may also use a promo code for payment
MYSportsEdTV is a community where athletes, coaches and parents connect and share their sport passion. We don’t sell our member data or send spam. Members will receive our FREE email newsletter to alert you about new video and blog content for the sports you follow.
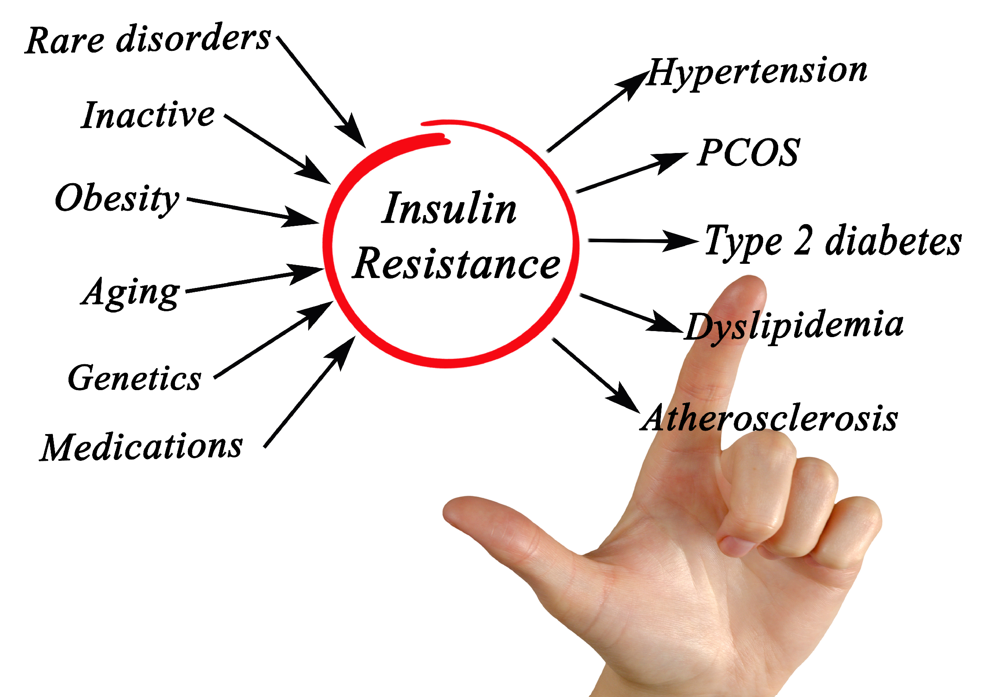
Insulin resistance is an increasingly common health issue, yet it remains poorly understood by many. It’s a condition where your body’s cells do not respond effectively to insulin, causing a cascade of health problems, including Type 2 diabetes, obesity, and cardiovascular disease. The good news is that insulin resistance can often be managed or even reversed with proper understanding and lifestyle changes. In this blog, we’ll break down the science of insulin resistance, its causes, symptoms, diagnosis, and what you can do to manage or prevent it.
What is Insulin Resistance?
Insulin is a hormone produced by the pancreas, and its primary role is to help cells in your muscles, fat, and liver absorb glucose (sugar) from the blood to use for energy. When you have insulin resistance, your cells don’t respond as well to insulin, so your body produces more to keep your blood sugar levels stable. Over time, this leads to an overworked pancreas and potentially Type 2 diabetes, as the body can no longer manage the elevated blood sugar.
Under normal circumstances, insulin works in a cycle:
- Glucose Enters the Bloodstream: When you eat, your body breaks down food into glucose, which enters your bloodstream.
- Insulin is Released: The increase in blood sugar signals your pancreas to release insulin, which helps glucose enter cells for energy or storage.
- Insulin Resistance Occurs when your cells don’t respond to insulin as efficiently. This leads to elevated blood sugar levels and an overproduction of insulin.
- Chronic Resistance: Over time, chronic insulin resistance can lead to prediabetes and, eventually, Type 2 diabetes.

The Relationship Between Insulin Resistance and Diabetes
While insulin resistance is not the same as diabetes, it’s a precursor to conditions like prediabetes and Type 2 diabetes. Here’s how it works:
- Prediabetes: This occurs when blood sugar levels are higher than normal but not high enough to be classified as Type 2 diabetes. It’s often the first sign that insulin resistance is advancing.
- Type 2 Diabetes: If insulin resistance continues and the pancreas can no longer produce enough insulin to regulate blood sugar, Type 2 diabetes develops.
- Type 1 Diabetes: While Type 1 diabetes is caused by an autoimmune response where the body attacks insulin-producing cells, individuals with Type 1 can also develop insulin resistance over time, especially if they experience high blood sugar levels frequently.
Who’s at Risk?
Anyone can develop insulin resistance, but certain factors increase your likelihood:
- Excess Body Fat, particularly belly fat (visceral fat), is highly associated with insulin resistance. Fat in this region produces inflammatory substances that can impair insulin sensitivity.
- Sedentary Lifestyle: Lack of regular exercise decreases insulin sensitivity, making your body less efficient at handling glucose.
- Diet: A diet high in processed carbohydrates, sugars, and unhealthy fats contributes to insulin resistance.
- Age and Genetics: Older age, a family history of diabetes, and certain genetic factors also increase the risk of insulin resistance.
- Hormonal Changes: Conditions such as polycystic ovary syndrome (PCOS) and Cushing’s syndrome can trigger insulin resistance.
Symptoms of Insulin Resistance
One of the challenges in diagnosing insulin resistance is that it often doesn’t cause noticeable symptoms until it progresses into prediabetes or diabetes. However, a few signs and symptoms may signal the development of insulin resistance.
Key Symptoms of Insulin Resistance
- Increased Thirst: When blood sugar levels are elevated, it can lead to dehydration, causing excessive thirst.
- Frequent Urination: As the kidneys work harder to filter excess sugar from the blood, this leads to increased urination.
- Increased Hunger: Despite high levels of glucose in the blood, cells aren’t getting the energy they need, leading to constant hunger.
- Fatigue: Insulin resistance prevents cells from efficiently using glucose for energy, causing chronic fatigue and low energy levels.
- Weight Gain, Particularly Around the Midsection: As insulin resistance worsens, it can cause weight gain, especially around the belly area, further exacerbating the condition.
- Darkened Skin: A condition known as acanthosis nigricans causes dark patches of skin, usually in areas like the neck, armpits, and groin. This is a hallmark sign of insulin resistance.
- Skin Tags: Small growths on the skin, often found in areas with friction like the neck or underarms, may be linked to insulin resistance.
- Blurred Vision: Elevated blood sugar levels can affect the lens of the eye, causing blurred vision.
- Slow-Healing Cuts and Infections: High blood sugar levels can impair the body’s healing processes, making cuts and infections take longer to heal.
- High Blood Pressure and Cholesterol Levels: Insulin resistance often goes hand-in-hand with elevated blood pressure and imbalanced cholesterol levels, which increases the risk of cardiovascular diseases.
These symptoms can develop slowly over time, making it easy to overlook insulin resistance until more serious health problems arise.
How is Insulin Resistance Diagnosed?
Since insulin resistance doesn’t cause obvious symptoms in its early stages, diagnosing it can be tricky. Healthcare providers typically use a combination of tests and evaluations to assess insulin resistance, including:
- Medical History: Providers will review your personal and family history of diabetes or related conditions.
- Physical Exam: Look for physical signs such as weight gain and darkened skin patches around the abdomen.
- Blood Tests: Several blood tests can help identify insulin resistance:
- Fasting Plasma Glucose (FPG): Measures your blood sugar after an 8-hour fast.
- Hemoglobin A1c (HbA1c): Provides an average of your blood sugar levels over the past 2-3 months.
- Lipid Panel: Measures cholesterol levels, as insulin resistance often leads to abnormal cholesterol.
- Glucose Tolerance Test (GTT): Checks how your body handles a glucose load by measuring your blood sugar over time.
While none of these tests specifically diagnose insulin resistance, they are commonly used to detect prediabetes or diabetes, both of which are closely linked to insulin resistance.
Managing and Treating Insulin Resistance
The good news is that insulin resistance can often be managed or even reversed, particularly in its early stages. The primary approach involves lifestyle changes, though medications may also be used in some cases.
Lifestyle Changes
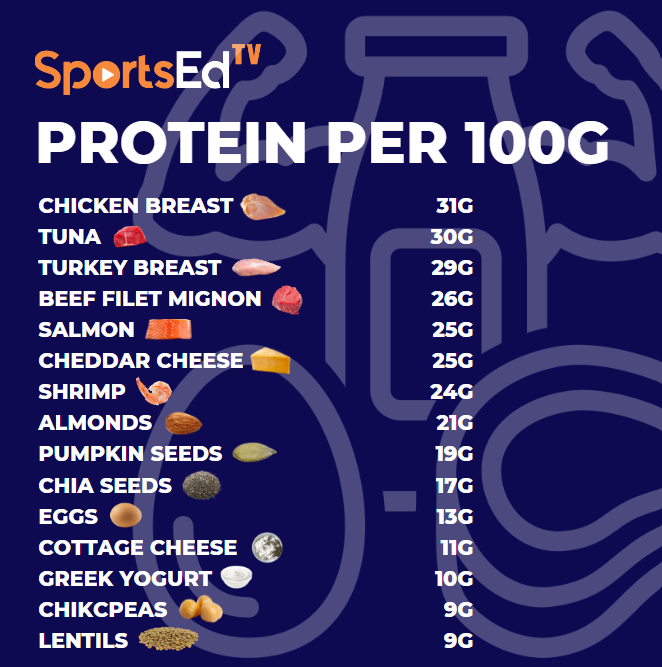
- Dietary Adjustments: One of the most effective ways to manage insulin resistance is through a healthy diet. Some key recommendations include:
- Focus on Low Glycemic Foods: These are foods that cause a slower, more gradual rise in blood sugar. Examples include whole grains, beans, vegetables, and most fruits.
- Avoid Refined Carbs and Sugary Foods: Foods like white bread, pastries, and soda can cause spikes in blood sugar, increasing insulin demand.
- Increase Fiber Intake: Foods rich in fiber, such as vegetables, whole grains, and legumes, help regulate blood sugar and improve insulin sensitivity.
- Choose Healthy Fats: Opt for unsaturated fats found in olive oil, nuts, seeds, and fatty fish like salmon, which are better for insulin sensitivity than saturated and trans fats.
- Exercise Regularly: Physical activity has a profound effect on insulin sensitivity. When you exercise, your muscles use glucose for energy, helping lower blood sugar levels and improving your body’s response to insulin.
- Aim for at least 30 minutes of moderate exercise most days of the week. Activities like brisk walking, cycling, or swimming can make a significant difference.
- Strength Training: Building muscle through resistance training can increase your muscle’s ability to absorb glucose, reducing insulin resistance.
- Lose Excess Weight: Even a modest weight loss of 5-7% of your body weight can improve insulin sensitivity. Losing weight around the abdomen is especially important, as belly fat is highly associated with insulin resistance.
Medications
While lifestyle changes are the cornerstone of managing insulin resistance, certain medications may be prescribed to help control blood sugar levels or manage related conditions. These can include:
- Metformin: Commonly used in Type 2 diabetes, metformin helps improve insulin sensitivity and lower blood sugar levels.
- Blood Pressure Medications: Insulin resistance often comes with elevated blood pressure, so medication may be needed to manage this risk.
Prevention: Can Insulin Resistance Be Avoided?
Prevention is vital when it comes to insulin resistance. While you can’t control all the risk factors (such as genetics and age), lifestyle choices play a major role in determining whether or not you’ll develop insulin resistance. Here are some steps to reduce your risk:
- Maintain a Healthy Weight: Excess body fat, particularly around the abdomen, is one of the biggest risk factors for insulin resistance. Keeping a healthy weight can prevent insulin resistance from developing.
- Eat a Balanced Diet: Prioritize whole foods over processed foods. Include plenty of vegetables, fruits, and lean proteins while limiting refined sugars and unhealthy fats.
- Exercise Regularly: Physical activity doesn’t just help prevent insulin resistance. It can also reverse early-stage insulin resistance. Try to stay active most days of the week.
- Get Enough Sleep: Sleep deprivation is linked to insulin resistance. Aim for 7-9 hours of quality sleep per night to help regulate blood sugar levels.
- Avoid Smoking: Smoking has been linked to insulin resistance and other metabolic issues, so quitting smoking can help lower your risk.

The Bigger Picture: Long-Term Outlook for Insulin Resistance
The long-term outlook for insulin resistance varies depending on how early it’s diagnosed and how well it’s managed. If caught early, lifestyle changes can significantly improve insulin sensitivity and prevent the progression to Type 2 diabetes. Many people can live with insulin resistance for years without ever developing diabetes, provided they take steps to control it.
However, if left untreated, insulin resistance can lead to a range of serious health issues, including:
- Type 2 Diabetes: Over time, insulin resistance can overwhelm the pancreas, leading to chronically high blood sugar levels and Type 2 diabetes.
- Cardiovascular Disease: Insulin resistance is linked to high blood pressure, high cholesterol, and other risk factors for heart disease and stroke.
- Metabolic Syndrome: This is a cluster of conditions, including high blood pressure, high blood sugar, and abnormal cholesterol levels, that significantly increases your risk of cardiovascular disease.
Living with Insulin Resistance
If you’ve been diagnosed with insulin resistance, it’s crucial to work closely with your healthcare team to create a plan that works for you. This may include monitoring your blood sugar levels, implementing dietary and exercise changes, and possibly taking medications.
Regular checkups are essential to ensure your blood sugar remains under control and to prevent complications from developing.
Insulin resistance is a complex condition with far-reaching health consequences if left unmanaged. But the good news is that lifestyle changes, such as improving your diet, increasing physical activity, and maintaining a healthy weight, can have a profound impact on insulin sensitivity. By taking action today, you can lower your risk of developing Type 2 diabetes and other serious health issues down the line. Always consult your healthcare provider for advice tailored to your specific situation. Taking steps now can lead to a healthier, more balanced future.