Tennis, Soccer, Health, Pickleball
Welcome and thanks for visiting...

Plantar Fasciitis – Part II

In the last article we talked about the anatomy of the foot, functionally how this helps to absorb shock and what the role of the plantar fascia is. This time, we will look at plantar fasciitis and how we can prevent and treat.
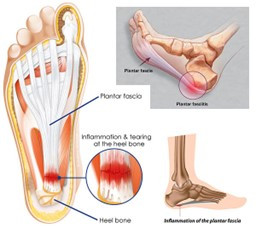
Plantar fasciitis is simply a swelling of the plantar fascia. This will happen when the load exceeds the capability of the tissue to resist, and the tissue responds by becoming inflamed. Plantar fasciitis can occur in any age of an athlete but is more common in our older athletes. With age, all our tissues become dehydrated. We see this in our hair, skin but also happens in the spine as well as the plantar fascia. A lot of older athletes will notice that their arches start to collapse after the age of 40-50. The arch collapsing is the result of a couple of things. One is decreased strength in the intrinsic muscles of the foot. With a decrease in strength of the smaller muscles of the bottom of the foot, they are not supporting the arch as much and the arch begins to fall. The second is decreased elasticity of the plantar fascia. With age comes a decrease in hydration of tissue. As tissues dry out and their flexibility or mobility is not maintained, these are not able to recoil as previous and tend to stay in a more lengthened position. This causes the arch to fall.
Typically, plantar fasciitis will start as a pin point area on the heel and can progress to the point where you are not able to bear weight on the foot. The key is early detection. As plantar fasciitis progresses, this can spread from pin point spot on the heal to becoming painful along the entire bottom of the foot and arch. The further the pain radiated from the heal, the more tissue that is involved and it gives you an idea if it is progressing or regressing in nature. The level of pain that is experienced can also indicate how much this is progressing or regressing. If the pain is a constant pain, this is more severe than a case where this is only pain first thing in the AM. Pain that is 1-2/10 at its most painful is a lot better than one that is at 8-9/10 at its most painful. Using these two simple concepts will let you know if you are getting better or getting worse.
Plantar fasciitis also has a common pain pattern. It is usually worse first thing in the morning when you go to step on it for the first time in the AM. As you sleep with your feet up and off the floor, swelling will accumulate in the area. Often when you go to step down first thing in the AM is when you get that sharp shooting pain. Plantar fasciitis is also progressive during the day. As you stand and move around in the day, it may go from a 1-2/10 in the AM to 6-7/10 pain at night. This makes sense since it is on the bottom of the foot and having to absorb a lot of stress during the day.
Some of the best preventative techniques are:


- Stretch as per above – these stretches should be held for 30-45 second each and NOT bounced. Hold at the end range of motion in a static stretch. – this will keep the tissue pliable and allow it to absorb more force without becoming irritated.
- Working you calves and anterior tibialis (anterior shin) with high reps and both eccentric training and concentric. - having good strength and endurance in these muscles will reduce excessive stress to the plantar fascia. If, for example, you have weakness of the anterior tibialis, when you run, this will cause your foot to slap the ground at heal strike. This foot slap creates excessive stress to the foot and can cause plantar fasciitis or shin splints.
- Work your intrinsic muscles of your foot. This is one thing that a lot of athletes don’t do. It is also the reason that a lot of martial artists don’t have plantar fasciitis as often as other athletes. Because they are bare foot so much in their sport and have to often use their feet to strike and control an opponent, you will see their feet are much more developed and resistant to development of plantar fasciitis.
Intrinsic strengthening is something we do a lot in physical therapy when someone presents with plantar fasciitis. One of the easiest ways to do this is to take a towel and place it on the ground. Place your foot on top of the towel and scrunch up the towel using your toes. This should be done with high reps (20-30 reps) or for an extended period of time (1-2 min). This can be progressed to doing this in standing. On a mat (like a wrestling mat) you can raise up on your toes slowly and let back down slowly. Then raise your toes off the mat coming back onto your heels. Return to starting position slowly then scrunch your toes into the mat. You can repeat that sequence 2-4 times for 20-30 reps per set or do for time.
One of the most common treatments we do is icing. Three techniques that I find very beneficial from the least aggressive to the more aggressive:
- Frozen water bottle. Freezing a plastic water bottle then putting under your foot and rolling back and forth around the painful area for 15 min is very beneficial. This can be done 3-4 times per day.
- Ice Massage – taking a paper cup, fill with water and freeze. Take the frozen cube out of the cup and perform as above or run directly on the foot for 5 min. This technique creates a layer of water between the skin and ice. This transduces the cold much more effectively and with tissues close to the surface is very effective. This will make a mess and should only be done for 5 min per session.

- Ice Bath – taking a bucket full of water and add ice till the temperature is between 45-55 degrees (no lower). Submerge your foot in this for 10-15 min. This is the most aggressive form of icing and is very effective for shin splints and plantar fasciitis.
Hopefully with some preventative techniques and treatment options, you can keep your feet healthy and avoid plantar fasciitis.
Read more:



